White blood cells are known to circulate through the entire body inside blood vessels, acting as a surveillance system. However, a specialized group of these cells are permanently present in tissues like the skin, intestine and lungs, protecting against external invaders, such as microbes. But it is largely unknown how these cells are generated. A new study led by Marc Veldhoen, group leader at Instituto de Medicina Molecular João Lobo Antunes (iMM; Portugal) and published this week in the prestigious Nature Immunology*, shows that the local availability of specific molecules is crucial to generate these tissue resident surveillance cells. The impact of these results extends beyond protective immunity in tissues, as these cells are also efficient when elicited after vaccination and yield more effective anti-tumor immunity.
These tissue resident surveillance cells are a specialized group of T-cells, important to directly attack invading microorganisms. “The tissue resident T-cells develop after an initial infection, as part of immunological memory, and provide protection against future infections”, explains Cristina Ferreira, first author of the paper.
Now, Marc Veldhoen and his team, have shown that within another population of T-cells, the regulatory T cells, mainly known for their ability to dampen immune responses to avoid damaging our own tissues, there are cells important for the development of these tissue resident T-cells. Using mouse models lacking this population of regulatory T-cells, the team observed that the number of tissue resident T-cells generated and present in the tissues was much lower. “It´s like the “surveillance system” in the gut, where we looked, was shut down. We could observe that a reduced number of the tissue resident T-cells resulted in less protection against invading pathogens”, explains Marc Veldhoen.
But what is the role of the regulatory T-cells in the development of the tissue resident T-cells? “What we observed is that the regulatory T-cells are alerted to move to the site of infection, where they promote the local availability of a specific molecule, TGF-beta. According to our results, this is crucial to generate the tissue resident surveillance cells”, explains Cristina Ferreira.
“We believe that learning more about how these cells develop might impact not only on how we look at infection conditions, especially in the gut, but also in cancer. It has been shown that the presence of tissue resident T-cells is important for a good outcome in cancer patients and, in animal models, studies have shown that these cells were most efficacious against cancer. Very likely, the reason is that these cells are specialized to penetrate deep into tissues. The more we know about these cells, the better we are equipped to develop ways to boost treatments in diseases, such as breast cancer”, adds Marc Veldhoen, on the importance of these discoveries.
This work was performed at the iMM (Portugal) with collaborations at Instituto Gulbenkian de Ciência (Portugal), Université Lyon (France), University Medical Center Mainz, Heidelberg University, and the German Cancer Research Center (DKFZ), Germany). This work was funded by European Union H2020 ERA project (No 667824 – EXCELLtoINNOV), Fundo iMM Laço, “la Caixa” Foundation and the Fundação para a Ciência e a Tecnologia (FCT).
*Cristina Ferreira, Leandro Barros, Marta Baptista, Birte Blankenhaus, André Barros, Patrícia Figueiredo-Campos, Špela Konjar, Alexandra Lainé, Nadine Kamenjarin, Ana Stojanovic, Adelheid Cerwenka, Hans C. Probst, Julien C. Marie and Marc Veldhoen (2020) Type 1 Treg cells promote the generation of CD8+ 1 tissue resident memory T cells. Nature Immunology. DOI: 10.1038/s41590-020-0674-9.
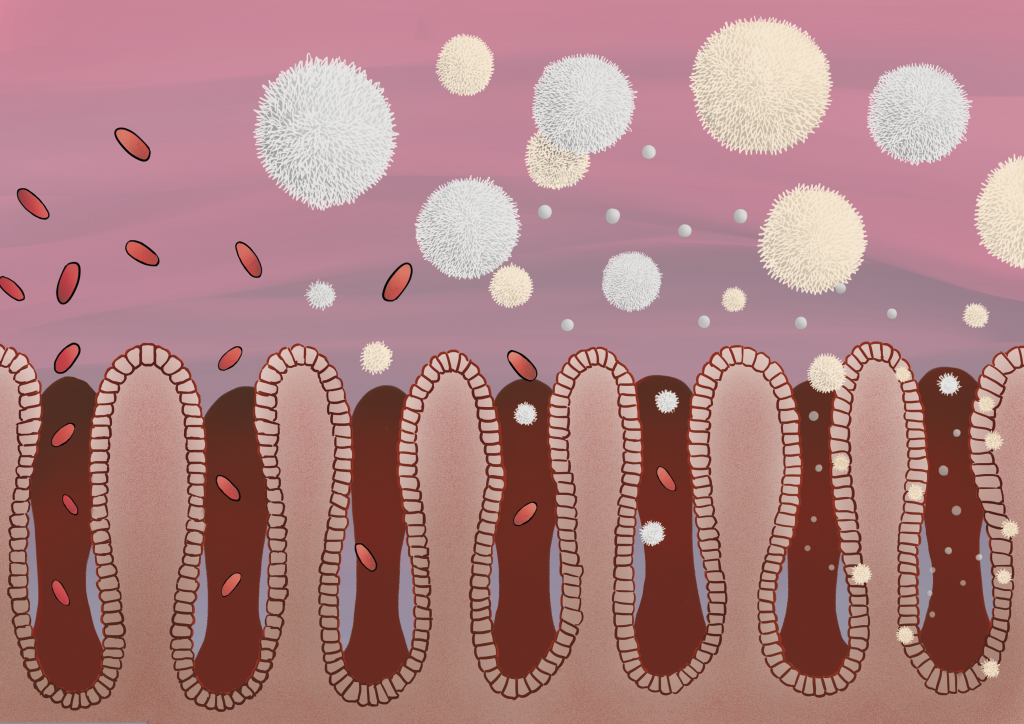
Caption: Regulatory T cells promote the generation of tissue resident T-cells in the intestine, essential for the protection against pathogens.
Credits: Helena Pinheiro, iMM