An international team led by Miguel Prudêncio at Instituto de Medicina Molecular (iMM; Portugal) together with Robert Sauerwein at Radboud University Medical Center (Radboud University Medical Center; Netherlands) and Perry van Genderen at Erasmus MC (UMC Rotterdam; Netherlands) published today in Science Translational Medicine, the results of a Phase 1/2a clinical trial of a potential new vaccine against malaria, named PbVac, involving a total of 24 healthy volunteers. While none of the vaccinated individuals was fully protected against disease, a remarkable 95% decrease in liver infection was observed in immunized volunteers relative to the non-immunized controls. This study paves the way for additional development of PbVac and similar vaccines for effective vaccination against human malaria.
Malaria is a disease caused by the parasite Plasmodium, which, despite tremendous progress made over the last decade, was the cause of over 400,000 deaths in 2018 alone. An effective vaccine against malaria is considered a crucial tool for prevention and future elimination of malaria. However, the clinical development of a malaria vaccine has proven to be a tremendous challenge for numerous research teams over the years and around the globe. The main reason for this arises from the complex biology of malaria parasites, which comprises multiple stages in both the mosquito and mammalian hosts, including an asymptomatic obligatory stage in the human liver.
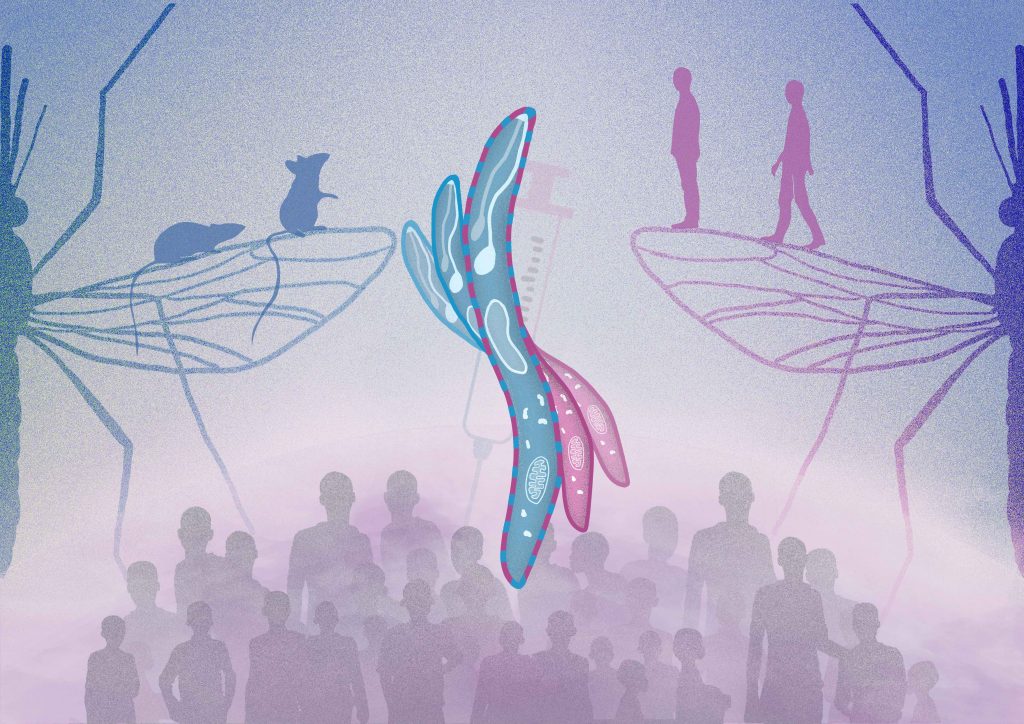
PbVac is the first member of a new class of agents intended for whole-organism vaccination against malaria. PbVac consists of a genetically modified rodent malaria parasite, Plasmodium berghei, which has been engineered to express a strongly immunogenic protein of its human-infective P. falciparum counterpart. Miguel Prudêncio, group leader at iMM (Portugal), explains: “This work started a few years back with this out-of-the-box idea of trying to use rodent parasites, that are not pathogenic to humans, as a basis for a new vaccine against malaria. Following the pre-clinical validation of PbVac’s immunogenicity and safety for human use, we have carried out, in partnership with colleagues at Radboudumc and Erasmus MC, and with funding and advice from PATH’s Malaria Vaccine Initiative, a first-in-humans Phase 1/2a clinical trial, involving a total of 24 healthy volunteers, to ascertain PbVac’s safety and protective efficacy in the clinic.”
The results now show that PbVac is safe and well-tolerated, and that it exerts a potent biological effect against infection by P. falciparum. The team observed a very significant 95% decrease in P. falciparum liver infection – the first stage of malaria infection in humans – in volunteers that were immunized with PbVac, when compared with control individuals.
Robert Sauerwein, whose team led the clinical assessment of PbVac at Radboud University Medical Center (Netherlands), says: “An effective vaccine is an essential part of a broad strategy in the fight against malaria. This approach shows that it works in principle, but that the composition of the vaccine or dose need to be adjusted”.
“We further showed that PbVac elicits the production of highly functional antibodies that recognize P. falciparum and significantly inhibit its ability to infect liver cells, further supporting PbVac’s potential for effective immunization against malaria”, adds Miguel Prudêncio.
For Perry van Genderen, “the use of this smart transgenic Plasmodium berghei sporozoite immunization platform has substantially widened the potential for development of new vaccines in humans”.
Miguel Prudêncio says: “This study provides clinical validation for this new approach to malaria vaccination, and opens possibilities to its optimization towards creating an effective vaccine against malaria.”
The pre-clinical work and the analysis of the immune responses was developed at iMM and the clinical assessment of PbVac took place at Radboudumc and Erasmus MC. This work was mainly supported by PATH’s Malaria Vaccine Initiative (MVI), and also by Fundação para a Ciência e Tecnologia, Portugal, Ministério da Ciência, Tecnologia e Ensino Superior (MCTES) through Fundos do Orçamento de Estado and the Dutch Research Council (Netherlands).
Today, in the same issue of Science Translational Medicine is published a second study on a different approach for a malaria vaccine. The major difference in the two approaches is that this vaccine uses a rodent malaria parasite that became more like the human variant through genetic modification, while the other study uses a human malaria parasite that became less harmful to humans through genetic modification. Amanda Fabra García, Geert Jan van Gemert and Robert W. Sauerwein, all from Radboudumc are authors in both studies.
Credits: Helena Pinheiro, iMM